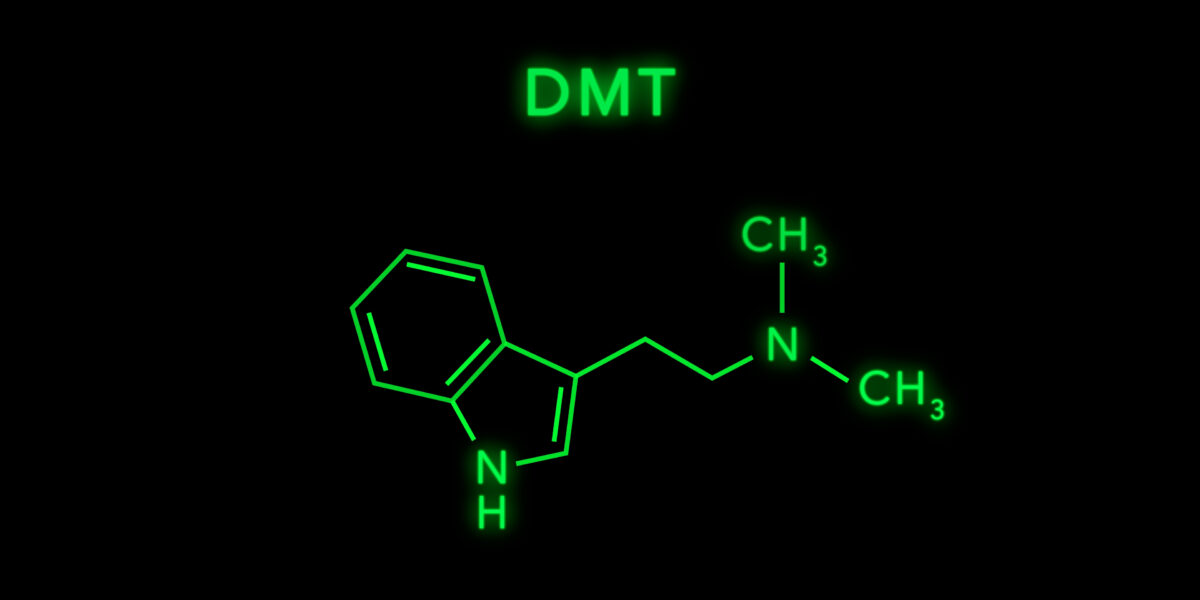
Many accounts of PIP centre on solipsism, death, and derealisation, which is an increasingly noted complication of psychedelic trips: a feeling that the world is alien and dream-like. One Reddit user, for instance, vapourised 5-MeO-DMT (toad venom) in search of an earth-shattering mystical experience – “I felt I was ready to meet God” – but instead was plunged into debilitating derealisation and depersonalisation (DP/DR) unlike anything he had ever known. “The outside world made absolutely no sense – what was once familiar became unfamiliar and alien.” His cognitive abilities were impaired: memory gaps (forgetting street names, not recognising his own home), difficulty speaking and forming thoughts, and a general sense that the drug had “wiped” part of his mind.
“It feels like I will never get out of it… it feels like I died,” he confessed, describing the episode as “the scariest experience of my life.”
Phenomenologist Klaus Conrad described the early phase of psychosis as “Trema”, a “delusional mood” where the world seems strangely charged with significance, or where the usual reality sense is altered: a commonly desired effect of the psychedelic drug. Patients may feel heightened meaning in trivial details, as if “something big” is happening. At this stage, there may be no clear false beliefs, only a pervasive sense that reality is “off.”
As this state intensifies, the mind seeks explanations, leading to an “apophany” or revelatory moment in which the strangeness is rationalised into a delusion – such as believing one is dead (Cotard delusion) or targeted by a conspiracy. Insight may initially remain, but it often fades as these interpretations solidify.
In one remarkable Reddit report, a user recounted being utterly convinced that he was dead or “that nothing else truly exists”. He simultaneously experienced other delusions (at times believing he was God or immortal) and a variety of hallucinations. The “walking corpse” belief proved impervious to family and friends’ reassurances – he thought others were figments of his imagination while he roamed in a sort of afterlife simulation. Tragically, this led him to a suicide attempt (to “escape from this reality/simulation”), after which he was hospitalised. With treatment, his Cotard’s delusion eventually remitted: after receiving antipsychotic therapy in the hospital, he reported being “hallucination-free and I believe that I exist and that I am alive”. (He wryly noted that the godlike delusion was harder to shake entirely, though greatly diminished.)
Another case, of a 16-year-old who developed long-term LSD psychosis, died by suicide while in a delusional state “because he didn’t think it would kill him”. LSD may pose a higher risk than psilocybin due to its longer duration, but the impact can be as severe. As one veteran put it, “It’s always a gamble… especially if you’ve already had psychosis once”.
Rather than merely feeling unreal, the psychotic may be so impressed by their affective state that they become convinced of their death/nihility. “My friend took mushrooms half a year ago”, one said. “He is convinced that he is not alive and is still in a trip. He still acts fairly normal in person but he keeps telling me that he believes he’s dead.”
Another anecdote comes from a Reddit user who had a bad LSD trip that planted a different unsettling idea: the notion that reality is a simulation, akin to The Matrix or The Truman Show, and people around him are “made up robots”. (It is worth noting that no less than Timothy Leary adopted a similar belief after his first LSD trip, after noticing the ways in which his speech and actions seemed to occur in a scripted behaviourist fashion in line with social mores. Equally, the popularity of ‘simulation’ must represent a quasi-intelligible response to broader existential or technological anxieties.)
After the trip, part of him truly believed his simulation theory and couldn’t shake it off. “It’s like 2 parts of my brain are fighting… One second I think it’s stupid to think this way, and the next I think it may be true because of what I saw during my drug experience,” he wrote, describing a tormenting back-and-forth between rationality and the bizarre conviction. The form of derealisation “I felt like I wasn’t real and everything was a simulation” one cannabis user said of a recurring episode.
Blogger Aella documented taking LSD weekly for 10 months (around 40 trips, often 150–400 µg each, with some up to 600 µg). As the experiment went on, she experienced a progressive detachment from reality and selfhood. She fell into a nihilistic, death-like mental state, whispering “I am dead” to herself and losing all desire and affect.
Rather than believing one is dead, the derealised subject may instead begin to believe that they are the only living person: solipsism. In a correspondence, a 35-year-old surgeon recounted a months-long descent into solipsism following heavy LSD use amidst a personal crisis. Initially prompted by an affair with a woman suffering from MDMA psychosis and BPD, his drug use spiralled into self-punishment and metaphysical unravelling. What began as emotional vulnerability metastasised into full psychosis, where he believed he was God in a solipsistic universe and attempted suicide to prove the reality of his beliefs. As he explained, “The altered state bled into sober life… I experienced the multiverse every waking moment.”
In responding to such cases, Adam Knowles, a psychedelic integration therapist and ayahuasca researcher, advocates ‘epistemological pluralism’ – opening interpretive space to the poetical meaning of their feelings, without categorising them simply as ‘delusions’. If a man believes he is Jesus, Knowles might ask, “Maybe Jesus is all of us?” Indeed, after the acute phase, many fall into a depression, feeling “lost” or fearing permanent brain damage due to self-stigma. “I feel like I gave myself brain damage and I’m never going to be the same”, one user wrote the day after his 5-hour psychosis (weed/LSD/DMT mix), perhaps reflecting the need to move away from a more passive brain-based understanding. Further, if the trip was terrifying, the person may develop symptoms akin to PTSD – nightmares, anxiety triggers (for instance, hearing a certain song that played during the trip might induce panic), intrusive delusional thoughts and memories of the trip’s most fearsome moments. Such a person may not be delusional per se, but extremely distressed and fearful that they could go crazy again, which paradoxically can feed into anxious paranoia.
There are innumerable flavours to the break from reality. One cannabis user literally begged his friend to crash the car they were in, “so we could crash and I could end my suffering”, because he believed he was irreversibly “mentally ruined” – demonstrating how the catastrophism of depressive thought may blur towards delusion. The commenter noted that subsequent use of a 70% THC cannabis strain led to panic and chronic depersonalisation. Another user, in a stimulant (crack) induced psychosis, said, “I almost committed suicide because I didn’t think it would end”.
A Reddit user shared a harrowing story after participating in an ayahuasca ceremony in Costa Rica. Like many others, her psychosis was not gradual but suddenly began with an extreme snap of anxiety and panic while intoxicated. Over the next 8 months, she said:
Intense energy sizzled through my body… My thoughts made me believe I was… trapped in hell for all eternity… I was… disconnected from life, my heart, and spirit… I ended up in the hospital from going manic and from constantly screaming that I was doomed for eternity… I was constantly planning my own suicide.
Similar somatic symptoms may occur without cognitive or affective changes. On psychedelic forums, long-time users acknowledge that unexplained shaking, seizure, and tremor episodes can occur with high doses of mushrooms or LSD. One experienced user called it “one of the mushroom world’s dirty little secrets… this happens all the time and there is no credible explanation for it”. The speculation in that community ranges from physiological causes like dehydration to psychological causes like conversion disorder (a stress-induced somatic reaction), but no consensus exists.
Even after recovering, some users report residual symptoms or an increased risk of relapse. In an online psychosis support forum, one commenter described how every subsequent drug use could thrust them back into psychosis after an initial LSD-triggered break. “Mine started with LSD, and eventually I couldn’t do anything [psychoactive] without going back into an episode… I’ve [been left with] lasting delusions that I can ignore or laugh off”, they wrote.
Yet it is worth distinguishing PIP from flashbacks, known clinically as Hallucinogen Persisting Perception Disorder (HPPD), in which a person experiences ongoing perceptual disturbances (tracers, afterimages, visual snow, etc.) for months or years after hallucinogen use. Yet Dr. Henry Abraham’s work documents patients whose visuals include grotesque or “devilish” figures otherwise found in more psychotic states. Here, the ‘meaning’ of the visuals is critical. A conventional psychiatric framing may risk estranging patients from their own percepts. When framed as evidence of “brain damage,” such a distance can become existentially corrosive. Faced with this dissonance, some reinterpret their visuals, folding them into mystical or occult worldviews.
Psychedelic-induced psychosis can be particularly insidious because the user may not realise anything is wrong. Psychedelics often engender mystical or spiritual sensations. “I didn’t know that I was psychotic – I thought I was having a spiritual awakening,” one individual admitted in retrospect. Indeed, psychedelics amplify the mind’s natural pattern-seeking tendencies, fostering the rapid formation of false or grandiose beliefs that may linger well beyond the acute experience. In a cultural landscape already saturated with unfounded conspiracy theories and loose spiritual syncretism – the “cultic milieu” described by Colin Campbell – such ideas can find ready-made interpretive frameworks that validate and reinforce them. In the digital age, the search to understand a strange experience almost inevitably leads online. Algorithms on YouTube, TikTok, and Reddit can steer a vulnerable person deeper into fringe ideas.
The looping quality of the psychedelic state may lend itself to later issues with tangential thinking. A recovering user noted his speech and thoughts were disorganised for a while. A mother described conversations with her psychotic son as “very weird” and full of non-sequiturs (like delusions about Elon Musk and Moses). “It’s been 4 months… my attention and memory are to the ground,” wrote one individual after a psychosis, worrying “I don’t know if I can have a job and family.” A Redditor recounts a harrowing weekend where a friend binged LSD and MDMA over three days, then eight years before. “He’s not even a shell of his former self… talking to him is like talking to a crazy person.”
A user on a psychonaut forum described a dramatic change in his longtime friend’s mentality after psychedelics. Over a year, the friend became “very interested and invested in a variety of conspiracy theories” to the point that “I’m convinced that he believes in [them].” He became convinced that the world would end in a couple of years, propagated the 432 Hz vs 440 Hz music tuning conspiracy, and subscribed to the flat-Earth theory. These were not ideas he held prior to using psychedelics. Additionally, this individual started exhibiting paranoid apocalyptic thinking (e.g. that an Armageddon is imminent) and identification with grandiose roles (he felt it was his mission to “preach” these revelations, and he almost considered himself a god). Family and friends grew alarmed as his behaviour became more radical. In this case, the duration has been over one year and is ongoing.











































share your toughts
Join the Conversation.