Psychedelics can provoke profound existential and spiritual experiences, which can be uplifting or deeply unsettling. In surveys of users with lasting difficulties, the most common themes were anxiety/fear, existential struggle, and derealisation. For example, Evans et al. (2023) found that 42% of respondents described “existential/ontological difficulties” (17% explicitly “existential struggle”) after their experience. Feelings of meaninglessness, loss of purpose, or derealisation were frequently reported. In colloquial terms, some describe this as a “spiritual emergency”. These effects often persist: about one-third had problems lasting over a year. Interestingly, the study found that prior mental illness did not statistically predict who got long-term difficulties.
If unresolved, these thoughts can spiral into depressive symptoms. Among a sample of 608 users, 12% developed prolonged depression after their bad trip, and about 6% experienced suicidal ideation. One participant recounted, “I collapsed into a severe, almost catatonic depression…fell further into the abyss of hopelessness and despair… I did not see the point. This lasted over 2 months.”
In a COMPASS Pathways trial of psilocybin (25 mg) for treatment-resistant depression, one participant (pseudonym “Zakara”) experienced a worsening of suicidal ideation that persisted for weeks. By the day after her session, she felt her life was “pointless” and that her death was “inevitable,” with constant, intensified suicidal thoughts (though no immediate intent). Four days post-dose, her depression hit “the worst she’d ever felt,” including impulses to visit train tracks (a place she had ideated about).
Another vivid account comes from a middle-aged Reddit user who took psilocybin mushrooms and experienced a nightmare trip. They described being “in a bright white space with ribbons of rotting flesh encircling me,” feeling utterly alone, convinced they might be “on another planet with no hope of returning home or seeing loved ones ever again.” This harrowing psychedelic vision of decay and isolation left a deep imprint. “Ever since then I have had anxiety with physical aches and pains and heavy depression about my own mortality,” they wrote. Prior to this, they said they were “never really been concerned about my own death” and had no history of anxiety or depression.
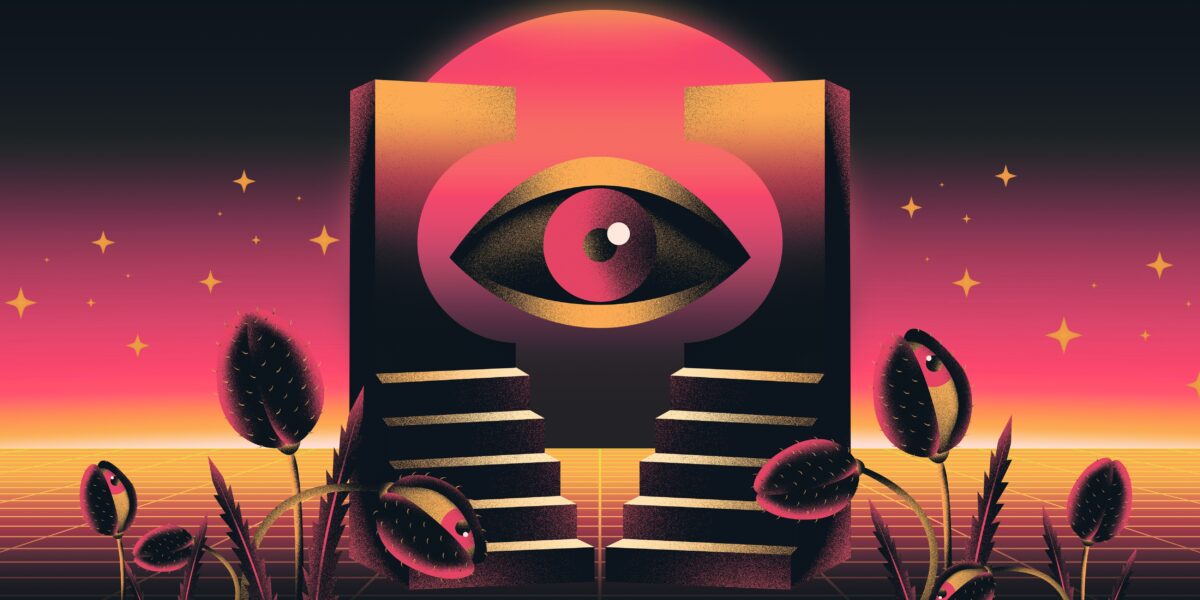
An Erowid report titled “Existential Crisis and Unwanted Ego Loss” (by user standsure, 2019) details a difficult LSD trip that led to profound nihilism. The user took three hits on a whim and was caught in rumination of “the force of ‘human conquest,’ strangling every last living beauty from this earth”, saying that they “contemplated suicide matter-of-factly (absent of terror and anxiety), while at other points [they were] seeing a divine eye and matrix overlooking me.”
“I realised that no matter what I did, there was no way to escape being a firm member of a destructive civilization. The notion that an environmentally destructive civilization is the ‘natural evolution of humankind’ became imprinted on my cosmic view.”
It is worth examining other psychedelic and related drugs. One ketamine clinic warns that “occasionally people experience a worsening of depressive symptoms and suicidality which persists for up to two weeks after taking ketamine”. Such reactions may be related to the mind-altering nature of the ketamine trance. If the patient is unprepared, this can feel like an “existential assault”. For instance, in a first-person account in The Washington Post, a patient described her initial ketamine session as “vacillating between existential dread and crippling anxiety” as buried emotions surfaced.
Classical ayahuasca research often emphasises its potential antidepressant effects. But large-scale data reveal that adverse mood reactions are not uncommon in the integration period. The Global Ayahuasca Survey (Bouso et al. 2022) collected data from over 10,000 ceremony participants worldwide. Strikingly, 55.9% of respondents reported some adverse mental health effects in the weeks or months after drinking ayahuasca. These were usually described as temporary depression, anxiety, confusion, or emotional turbulence during post-ceremony integration. Most (≈88%) of users interpreted these difficulties as “part of a positive growth or integration process” rather than a purely harmful effect. Still, 12% felt the need to seek professional help for their post-ayahuasca mental struggles.











































share your toughts
Join the Conversation.